Gene therapy breakthrough offers hope to children
1 Jul 2021, 3 p.m.
Scientists and doctors have given hope of a gene therapy cure for children with a rare degenerative brain disorder called Dopamine Transporter Deficiency Syndrome (DTDS).
The team of reseachers are from University College London Great Ormond Street Institute of Child Health (UCL GOS ICH) and Great Ormond Street Hospital (GOSH).
The results of the study are so promising that the UK regulatory agency MHRA have advised the researchers that they can now prepare for a clinical trial.
Professor Manju Kurian, co-lead author of the study, discovered the disease in 2009.
GOSH Charity granted her seed funding worth just over £86,500 to begin developing treatment.
“Our study provides real hope of an effective treatment for children who are living with this devastating, life-limiting brain disease, and it is hugely exciting to be at the stage of planning a clinical trial just ten years after discovering the gene that causes the condition.”
What is DTDS?
DTDS was discovered by Professor Manju Kurian in 2009.
It's a rare, progressive and life-limiting neurological condition caused by a faulty gene that affects brain cells.
Infants with DTDS are rarely able to learn to walk or speak. As they grow, they develop ‘parkinsonism’ - so called because of similarities to Parkinson’s Disease. This includes slow movements, involuntary twisting postures of their arms and legs and whole-body stiffness.
There are currently no effective treatments or a cure. Most children with DTDS sadly die before reaching adulthood, often from respiratory infections or other complications.
The condition is rare, with 50 children worldwide currently known to doctors. It has previously been mistaken for cerebral palsy and may continue to be undiagnosed.
How does the precision gene therapy work?
Scientists took skin cells from children with DTDS and turned them into stem cells, which can grow into any type of cell to build or repair different parts of the body.
Professor Kurian’s team, with work led by Dr Serena Barral, converted these stem cells into the exact brain cells (dopaminergic neurons) that carry the genetic ‘fault’ responsible for DTDS.
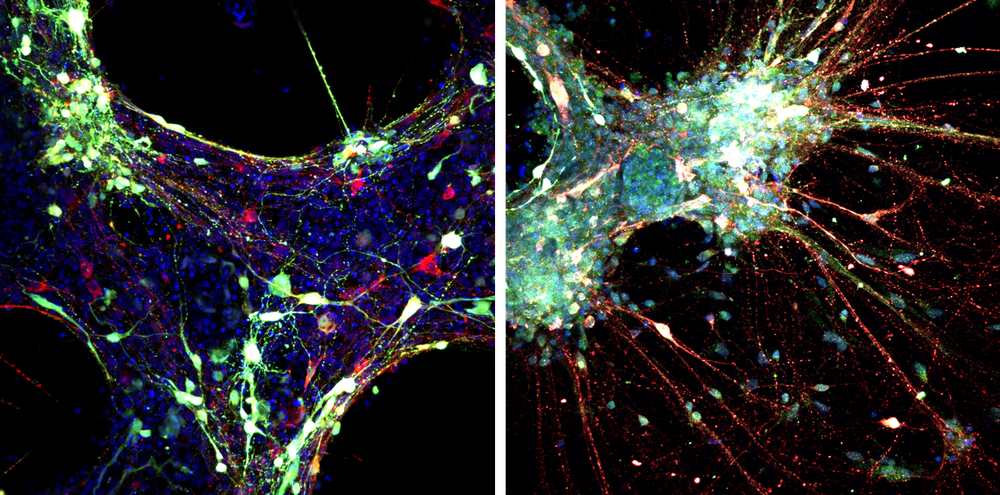
Using this laboratory model – or ‘disease in a dish’ – made directly from the cells of children with this rare condition, scientists were able to test the experimental gene therapy for DTDS and show that it could relieve the disease-related defects in DTDS brain cells.
The team used fluorescence microscopy to see what was happening in their ‘disease in a dish’. The image on the left shows how neurons and their communicating ‘arms’ had not formed properly in cells with DTDS. The image on the right is of gene therapy treated cells, and shows the DTDS cured in a laboratory model.
A further collaboration with UCL’s Professor Simon Waddington and Dr Joanne Ng enabled the researchers to study DTDS in mice and test gene therapy as a cure.
The gene therapy injects a modified, harmless virus containing the healthy gene into the area of the brain where this gene is missing.
The mice were successfully cured of their symptoms including involuntary and disordered movements, progressive parkinsonism and weight loss.
Based on the promising results of the laboratory tests, the next phase is to develop a clinical trial which would involve children diagnosed with DTDS.
The research team will be based at the Zayed Centre for Research into Rare Disease in Children, which is a partnership between GOSH, UCL, and GOSH Charity.
It's hoped the clinical trial will launch at GOSH.
Meet Shannon

22-year-old Shannon from Cornwall was one of the first patients diagnosed with DTDS after Professor Kurian discovered the faulty gene in 2009.
Her mum, Judith, said: “Shannon is a happy, bubbly girl and finds everything hilarious. DTDS meant Shannon suffered badly from shakes - she couldn’t control her legs. She shakes very slightly now, but it’s very mild.”
On Shannon being one of the first patients in whom the faulty gene was discovered, Judith said, “It’s amazing. The last time we saw Professor Kurian she said there had been a breakthrough with the research, but it hadn’t been tried on anyone yet.
“GOSH is a brilliant hospital and I donate to the charity every month to help keep the extra support at the hospital going.”